LIFT
Longitudinal Integrated Foundation Training (LIFT)
LIFT I: 2016 - 2018
LIFT 1: 2016 – 2018 (Pilot)
The 2012 Broadening the Foundation Programme Report was aimed at broadening trainees’ exposure across a breadth of health services and encouraging training initiatives away from purely hospital environments. One of these initiatives was the development of integrated placements between acute and community which have since struggled to advance in favour of more traditional training models in the vast majority of NHS services.
The modern NHS is a rapidly changing environment and our training models need to adapt and evolve to equip the doctors of the future with the skills and attributes they need to respond to the changing healthcare needs of society.
In the current foundation training environment we’re accustomed to the notion of trainee, trainer and patient having a symbiotic learning relationship is easily lost and there is a considerable body of literature commending longitudinal training, with evidence for better training and better clinical care, as an approach to unify these connections.
In the United States, the work of Prof David Hirsh and others has shown great value in the continuity of integrated training through longitudinal clerkships and the detrimental effect of compartmentalised attachments.
David Hirsh discusses the benefits of longitudinal clerkships
https://www.youtube.com/watch?v=cKGeWSws1So
In collaboration with Prof David Hirsh the North West of England Foundation School piloted a number of Longitudinal Integrated Foundation Training (LIFT) programmes in the 2016 across 8 acute trusts;
- Wigan
- East Lancashire
- Wirral
- Stockport
- South Manchester
- Morecambe Bay
- Pennine Acute
- Bolton
The LIFT programmes did not have a traditional four-month FY2 placement in General Practice but instead had 6 four-month placements in acute specialties with a longitudinal attachment to a practice for the duration of the two-years.
All of the LIFT programmes were rich in clinical experience and provided the expected standards of teaching and learning, as well as clinical and educational supervision with longitudinal competency themes such as values, leadership, self-management, patient safety and quality improvement continuously targeted and tracked. The doctors produced were well-versed in patient-centred care across a range of care pathways.
The school hosted 3 regional development days throughout the pilot for the trainees, trainers and faculties involved with LIFT to share best practice and learning, and the programmes themselves were independently evaluated by consultant psychologists throughout the two-years.
The following comments were captured from the trainer and trainee evaluation reports and illustrate some of the perceptions and themes which came out.
Trainer Perceptions of LIFT
Supervisors comment on the trainees’ ability to treat patients “holistically” and how they excel at such as providing essential referral and hospital discharge information.
The longitudinal relationship affords GPs the opportunity to get to know their trainees sufficiently to enable them to “challenge” trainees in ways they would not usually feel able. Some GP supervisors comment that they themselves have gained from LIFT as much as the trainees, benefiting from the relationship, gaining experience and developing their own training skills in ways not possible with trainees on a shorter placement.
GP supervisors have “enjoyed seeing the trainees develop” and following their “transition from medical student to doctor”. They have found this “fulfilling”. Several GP supervisors discussed how sorry they will be to lose their LIFT trainees when the pilot ends, having now built close relationships.
Trainee Perceptions of LIFT
The time spent in primary care was one of the most positive aspects of the LIFT programme. Participants reported improved communication and consultation skills, a greater ability to deal with complex, diverse and uncertain situations. The trainees’ growing sense of independence and confidence in primary care was also facilitated by permission to prescribe and conduct more autonomous consultations in FY2.
Many participants described how their experience on the LIFT programme had enabled them to see “both sides” of the care pathway, develop a better understanding of the options available and ways to improve the efficiency and continuity of care between the sectors. Participants also reported being able to transfer and apply their knowledge between their placements.
Time in primary care nurtured a more holistic view of the patient, enabling a closer understanding of the patient journey and the development of good patient relationships. There was broad agreement that this experience had enabled them to become more ‘well rounded’, ‘patient-centred’ doctors in comparison to their secondary care colleagues. Relatedly, participants reflected an increased respect and recognition of the GP’s role counter to a general cultural bias against GPs manifest in the hospital setting.
A number of additional quantitative and qualitative surveys were carried out during the pilot to evaluate preparedness for progression and wellbeing, versus traditional training programmes.
The following are some of the key findings from these additional surveys;
- Proportionately more LIFT trainees entered specialty training vs non-LIFT trainees. 57% entered specialty training without deferring. This compares with 38% of standard trainees.
- Proportionately more LIFT trainees entered General Practice vs non-LIFT trainees. 50% of LIFT trainees choose GP training without deferring. This compares with 32% of standard trainees.
- 92% of LIFT trainees rated their “ability to make an informed career choice” as ‘high’ as opposed to 72% of standard trainees.
- LIFT trainees felt more valued, supported and satisfied in their roles
- LIFT trainees had a lower sickness absence rate
- LIFT trainees tended towards more compassionate reflections
Fig 1 shows the comparison of LIFT trainees vs standard trainees over 3 areas of wellbeing using the psychometric Maslach Burnout Inventory; Emotional Exhaustion, depersonalisation and personal accomplishment. On all three accounts the LIFT trainees reported more favourably
(Fig 1)
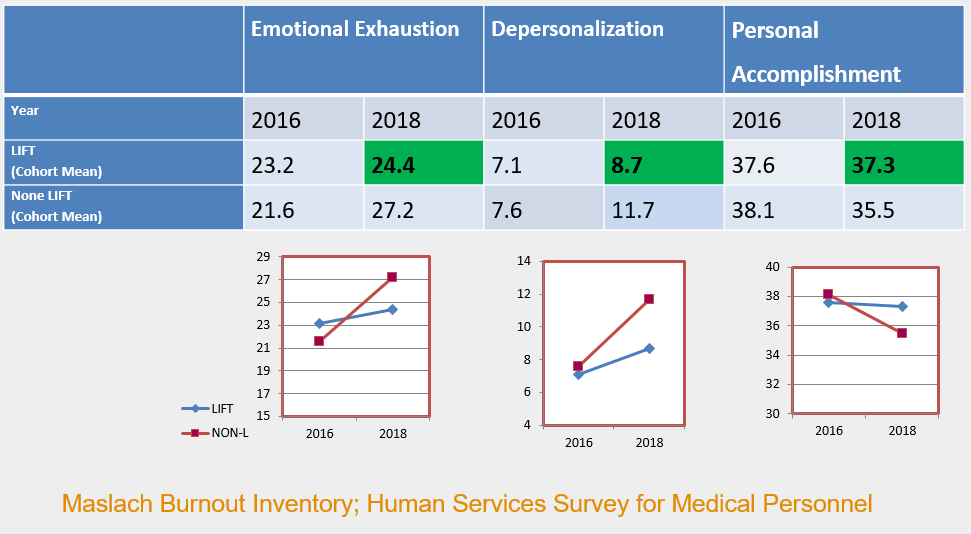
Fig 2 shows the comparison between LIFT trainees and standard trainees on the number of days out of programme (sickness rate) and the number of significant events recorded on the Form R. When scaled up proportionately this shows that LIFT trainees reported 522 less patient safety issues and saved 4,194 working days from sickness absence.
(Fig 2)

In regards to knowledge and support;
- 100% of LIFT trainees rated their “understanding of how primary and secondary care work together in the NHS” as high, compared to 78.6% of standard trainees
- 83.4% of LIFT trainees reported that they had been well supported pastorally/personally in the workplace compared to 71.3% of standard trainees
- 100% of LIFT trainees reported that they felt well supported educationally in comparison to 72.8% of standard trainees.
A suite of guidance documents was produced to accompany and support the pilot and can be found below for information:
Guidance for the supervision of F1s in GP